Considerations on the Hruska Adduction Drop Test
Michael J. Mullin, ATC, PTA, PRC
The Hruska Adduction Drop Test (HADT) is one of the most recognized and universally utilized assessments of the Postural Restoration Institute® It provides very valuable information of the orientation and integrity of the hip on pelvis, in particular the AF/FA orientation. It is a position test which helps to determine pelvis neutrality, joint centration of the femur on the acetabulum and aberrant soft tissue tone. Suboptimal positioning of the femur in the cotyloid acetabulum, on one or both sides, produces poor force coupling and renders the involved hemi-pelvis vulnerable to further dysfunction. Pain, injury, decreased function or performance may occur as a result. When performed correctly, it should be one of the stalwart tools in the PRI practitioner’s toolbox, and for many reasons other than just as the test. As one becomes more adept at performing the HADT, the set-up, quality of movement, and the end-feel can provide the practitioner with other useful pieces of information. While some of the added observations are more subjective and empirical in nature, they still provide valuable insight into the state of the pelvis in general. Accessory and aberrant movement, general underlying soft tissue tone, the degree of spine involvement and even possible underlying damage to the joint can be gleaned out, in particular when correlated with other test findings. The following are some thoughts and observations on optimizing success with performing the HADT and what other information this powerful assessment can provide.
The HADT as a positional test
- There are some subtleties which seem to make a difference in the quality of the results.
- “The patient lies on his or her side with the lower leg and hip flexed (90°). Stand behind the patient and passively flex, abduct and extend the top hip to neutral while maintaining 90° of knee flexion.”
- If you’re struggling to keep the top hemi-pelvis stabilized and/or if the patient has difficulty relaxing the leg, it is likely positive.
- If the lower leg has a difficult time staying bent at 90 degrees and starts to extend while you move the top leg, it is likely positive.
- Remember that when “extending the hip to neutral”, that this is relative to the top pelvis position during set-up, so strictly using the plane of the body as a guide to determine 0° or “neutral” may likely be different depending on which side is being tested. Getting the Right hip to neutral might mean that the Right leg shouldn’t necessarily get to the plane of the body as much as the Left does before adducting. This is due to the position of the acetabulum with the Right side already being extended more than the Left side.
- “Passively stabilize the pelvis from falling backward and allowing femoral internal rotation to occur.”
- It is better to get your body right behind the top pelvis to help stabilize it in order to make sure it does not roll back. Care should be taken not to lean too much into it, thus biasing the pelvis into a forwardly rotated position as a result. This is accomplished through varying levels of stabilization, depending on the patient and the size and strength of the practitioner.
- It’s easy to let the femur IR. Don’t let it. . .
- “The patient lies on his or her side with the lower leg and hip flexed (90°). Stand behind the patient and passively flex, abduct and extend the top hip to neutral while maintaining 90° of knee flexion.”
www.posturalrestoration.com
- “Make sure the top innominate is positioned directly over the bottom innominate so the frontal plane starting position does not give any false positives (top innominate too cephalad) or false negatives (top innominate too caudal).”
- Remember that it is likely that the Right and Left sides will need to be set-up and stabilized a little differently to make sure of proper hip stacking.
- A Left sidelying person for a Right leg test will likely have to have their Right hemi-pelvis stabilized from laterally tipping or rolling back, especially if a strong pattern.
- A Right sidelying person for a Left leg test will likely have to have hemi-pelvis stabilized from anteriorly rotating more than its current resting position and from their thorax abducting/adducting. Care should be taken to not let the pelvis anteriorly tip (more) or for the back to extend (more).
- Remember that it is likely that the Right and Left sides will need to be set-up and stabilized a little differently to make sure of proper hip stacking.
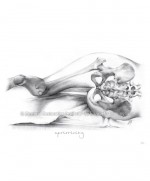
Positive HADT Negative HADT
Illustration by Elizabeth Noble for the Postural Restoration Institute®. Used with permission ©Postural Restoration Institute® 2014. www.posturalrestoration.com
- “A positive result is indicated by a restriction from the anterior-inferior acetabular rim, transverse ligament, and piriformis muscle or impact of the posterior-inferior femoral neck on posterior inferior rim of the acetabulum; possibly secondary to an anteriorly rotated, forward hemipelvis. Usually seen on the left, especially if left Extension Drop Test is positive in a Left AIC oriented patient.”
- False negatives can occur easier than false positives, and as a result can greatly affect subsequent treatment hierarchies. Taking time to really make sure the set-up position and execution of the test is performed optimally is critical.
- It is not uncommon to have to execute it a few different times if the practitioner is at all unsure if they have achieved an accurate result.
- Stabilization of the top part of the hemi-pelvis is crucial and will often need to be stabilized with more or less pressure depending on the side performing it on, the position of the pelvis or how strong the pattern.
- The top hand is doing more than just stabilizing. It assessing what is happening with the top pelvis and femur in terms of accessory movement.
- Perform the test and if at all unsure, roll the pelvis a little forward and perform again, then roll it back a little and compare each result. This is where the quality of movement and end-feel assessment is helpful.
- This is also where comparing these findings to other test results is key.
- For people who have larger hips, they may not get all the way to the table, on either side, when examining them and that doesn’t mean they are automatically a PEC.
- There is a spectrum of results in any assessment other than just positive or negative, but the ability to differentiate between some of the results takes practice with performing it a number of different times on a number of different body types, much like any other orthopaedic special test.
The following examples outline other pieces of information that the HADT can provide:
The HADT as an evaluative aid of the quality of both the AF and FA motion
- The ease or difficulty of trying to get the person into position to perform the assessment, the challenges with the patient remaining relaxed while performing, and what the patient tried to do while performing the assessment are valuable clues about what else might be going on.
- It provides the practitioner feedback about how strong of a pattern they have.
The HADT as a teaching tool for the patient/client
- After performing the test the first or second time on the person—showing the before, positive result, and then after repositioning, a negative result—they have an improved appreciation of what the goals are for balanced position. They can feel and appreciate the difference.
- Home program compliance improves dramatically.
- When used with the Pelvic Ascension Drop Test, someone can get an idea on their own if they are maintaining good position.
www.posturalrestoration.com
The HADT as an assessment of possible underlying hip pathology
- While performing the HADT, patient symptomatology such as pain, pinching, snapping, or catching and practitioner assessments such as bony end-feel, crepitus or grinding, can all suggest the involvement of underlying intra-articular damage or other pathology.
- It is also important to point out that even though the Right hemi-pelvis may have a negative result—in particular after techniques have been employed to reduce a PEC pattern—that this does not mean that the Right side is in an optimal position either. A negative result merely means that the hip can adduct. However, there may be so much adduction and internal rotation on the Right that it may have stretched out the superior aspect of the iliofemoral ligament and capsule.
- In the realm of PRI tests, a negative result is not always a good thing, in particular with a more open end-feel in the finish position. One can be over-negative, and it’s called patho.
In conversations with people and in response to things I have read, a comment I have heard a few times is: “It seems like at times you’re trying to make it a positive result on the Left.” The reality is, yes, you are. Meaning, if it’s there, you want to find it. The treatment hierarchy is established based on certain criteria having been met before progressing. Patient responses and outcomes will also be affected if proper position is not attained before progressing.
The following are other practical uses of the HADT:
- To help determine if someone is in the correct shoes and even to see if they are tying their shoes correctly. You can have someone come in with new shoes and HADT them before, and then after wearing the shoes to see if it changed the results.
- However, this is only one piece of the puzzle, and the results may not affect HADT but may affect other findings (i.e. HG IR, horizontal abduction) and visa versa.
- When utilized as a measurement of position with visual integration strategies, it can help determine if improved ambient, peripheral processing has been established.
- It is a great education tool for the patient/client as to why they should be doing their home program due to the changes in test results after they perform certain activities.
- At the end of a treatment or training session, it is good to use this as a quick check that the person maintained their neutrality with the program you outlined.
- During rehab, it can also be used to see if during a session some of the repositioning activities are being performed correctly or that they are doing the most appropriate ones. It can help establish if more consistent repositioning activities are necessary until all factors have been addressed and adequate neural plasticity has been established.
- During performance training, weight training, and with some athletes, you likely won’t want to have them being “neutral” during their whole activity. The most important part is that they can come back out of a higher, sympathetic state after activity to be able to rest and recover.
This is by no means an exhaustive list of the benefits of the HADT. Much like many of the PRI tests, it holds a bounty of uses above and beyond what it is listed for in the course manual, as well as provides valuable insight into what your patient/client’s presentation and needs are.
FOR FURTHER INFORMATION
- www.posturalrestoration.com
- PRI course manuals: Myokinematic Restoration, Pelvis Restoration, Postural Respiration
- Tenney HR, Boyle KL, DeBord A. Influence of Hamstring and Abdominal Muscle Activation on a Positive Ober’s Test in People with Lumbopelvic Pain. Physiotherapy Canada 2013; 65(1):4-11.